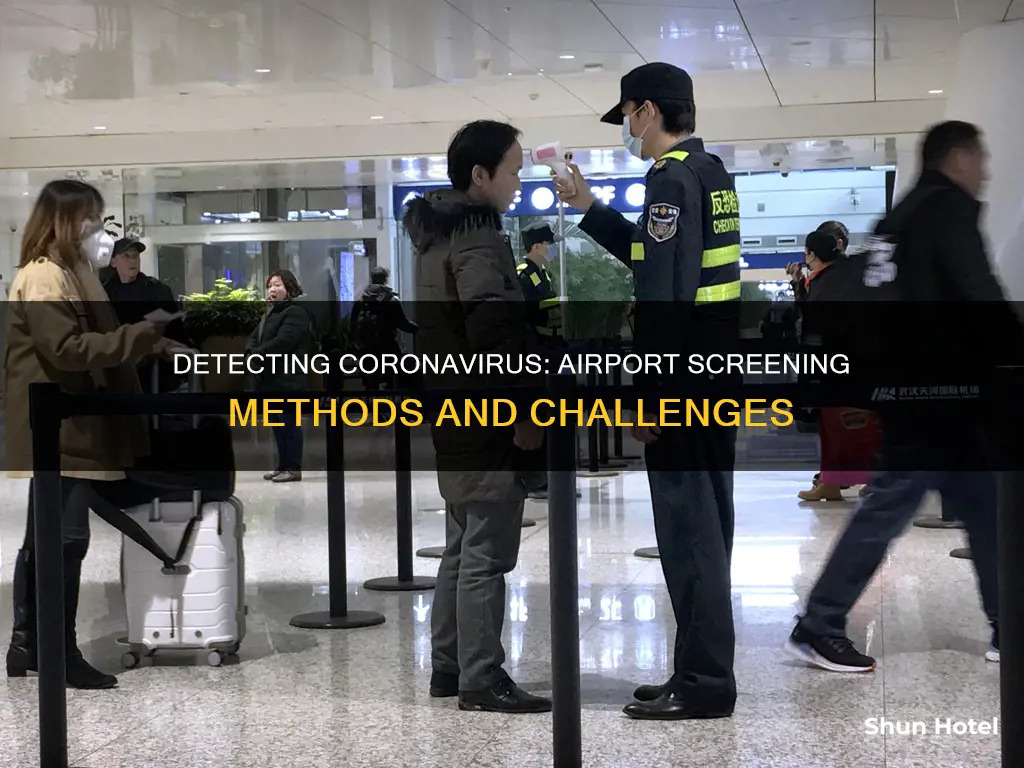
Detecting coronavirus at airports has been a key concern for governments and health authorities since the early days of the pandemic. Airports have implemented various measures to detect coronavirus, including temperature checks, health questionnaires, and thermal cameras. However, the effectiveness of these measures has been questioned, especially given the long incubation period of the virus and the possibility of asymptomatic cases. While these procedures may help reassure the public, there is little evidence to suggest that they are making a significant difference in detecting infected travellers.
Thermal screening, in particular, has been controversial. It was widely implemented during the 2003 SARS epidemic and later during the 2009 bird flu epidemic. However, it has not proven entirely accurate, as it may flag passengers with different types of infections while missing those who are incubating the virus but have not yet developed symptoms. According to a study by the London School of Hygiene and Tropical Medicine, out of every 100 infected travellers on a 12-hour flight, 42 would pass through both entry and exit screening undetected.
As an alternative, some airlines have started offering coronavirus tests for passengers before boarding, either through kits mailed to their homes or rapid tests taken at or near airports. However, these tests are not 100% accurate, and there are concerns about the availability of rapid tests and the potential for increased gridlock at airports. Overall, while efforts to detect coronavirus at airports are important, they should be combined with other measures such as contact tracing, rapid self-isolation, and public health education to effectively control the spread of the virus.
| Characteristics | Values |
|---|---|
| Screening method | Thermal cameras, temperature-scanning cameras, handheld infrared thermometers, ear gun thermometers, full-body infrared scanners, molecular tests, antigen tests |
| Effectiveness | Thermal screening is controversial and may not always be effective at detecting early signs of infection. It may flag up passengers with a different type of infection, while missing those who are incubating the virus but have not started to show symptoms yet. |
| Drawbacks | The timing of the Covid-19 outbreak coincides with the peak flu season in Europe and China, so thermal screening may not be the best method. |
| Alternatives | Quarantining measures, providing information on how to reduce the risk of transmission, basic health information |
What You'll Learn

Thermal cameras can detect elevated body temperatures
Thermal imaging cameras are an effective way to detect elevated body temperatures, which is one of the first and most important indicators of a coronavirus infection. Airports around the world have been using these cameras to screen passengers for coronavirus symptoms.
Thermal cameras such as the XC300 and XC600 from Trotec use an acoustic IR screening alarm to detect elevated skin temperature in individuals, even in large crowds. The cameras are set to a predefined alarm value, for example, 38°C, and will sound an alarm if this normal temperature is exceeded. This method is completely contactless, measuring the skin temperature at a convenient distance above the forehead of the person being examined.
The use of these cameras has been implemented in airports such as Los Angeles International Airport, which began testing temperature-scanning cameras on passengers in June 2020. Istanbul Airport also used thermal cameras to scan passengers arriving from Far East countries as part of Turkey's Health Ministry's measures against the coronavirus outbreak.
While thermal cameras are a useful tool for early detection, it is important to note that they do not detect coronavirus infections directly. Instead, they detect changes in skin temperature, which may be caused by other factors such as physiological stress. Further examinations by trained medical personnel are necessary to confirm a coronavirus infection.
Ann Arbor Airport: Does It Exist?
You may want to see also

Handheld thermometers can be used for exit screening
Handheld thermometers are just one tool that can be used for exit screening at airports. Other methods include full-body infrared scanners and ear gun thermometers. These methods also have limitations and may not detect all infected individuals. For example, some individuals may have a mild case of the virus and not exhibit any symptoms, even at their peak.
It is important to consider the advantages and disadvantages of using handheld thermometers for exit screening. On the one hand, they can help identify potentially infected individuals and prevent them from boarding a flight. This can reduce the risk of transmission and protect other passengers and crew. Additionally, handheld thermometers are portable and easy to use, making them suitable for busy airport environments.
On the other hand, handheld thermometers may not detect all infected individuals, especially those who are asymptomatic or in the early stages of infection. Additionally, the use of handheld thermometers can be time-consuming and may cause delays at airports. It is also important to ensure that the devices are properly calibrated and used correctly to obtain accurate readings.
Overall, while handheld thermometers can be a useful tool for exit screening at airports, they should be used in conjunction with other measures to effectively detect and prevent the spread of coronavirus. This may include providing information to passengers on symptoms and recommended actions, as well as implementing quarantine measures for those who are suspected or confirmed to be infected. A combination of strategies will help reduce the risk of transmission and protect the health and safety of travellers and staff.
Airport Security: What Can You Bring?
You may want to see also

Quarantining measures are scientifically effective
Quarantining measures are scientifically very effective. The US military has set up 11 quarantine camps next to major airports, which can accommodate up to 250 people each. A hotel at Heathrow Airport has also been block-booked to serve as a potential quarantine zone for people entering the UK with symptoms. In the case of Hawaii, the state requires all visitors to either quarantine for 14 days upon arrival or show a negative result from a recent coronavirus test.
Quarantining is effective because the person is isolated for the entirety of the potential incubation period. The incubation period of the virus can be as long as 14 days, with an average incubation period of 5.2 days. During this time, some cases are mild and may not show symptoms even at their peak. Therefore, quarantining for the full 14 days ensures that even those with mild or asymptomatic cases will not spread the virus.
Furthermore, quarantining can be combined with other measures to increase its effectiveness. For example, in the United States, passengers arriving from China receive a card informing them of the symptoms to watch out for and advising them to take their temperature twice a day. This has proven effective, as in one case, a man who was asymptomatic at the airport and passed the screening checks became ill the day after returning home. After consulting the card, he followed the advice to stay at home and contact his local health department.
San Francisco Airport: Fire Impacts and Safety Measures
You may want to see also

Testing kits can be mailed to passengers' homes
Testing kits are also available for purchase from pharmacies, such as CVS, which offers a range of at-home COVID-19 test kits, including the CVS Health At Home COVID Test, BinaxNOW, Ellume, Pixel, and QuickVue. These tests may be fully covered by insurance, so passengers should check with their insurance provider.
At-home testing is a useful way to get results if travellers are concerned that they may have contracted COVID-19, either before or after their journey. Testing kits can be purchased and performed by the traveller themselves, with results available in under an hour for antigen tests, or several hours to days for PCR tests. Testing kits will include everything needed to complete the test, and passengers should carefully follow the instructions provided. Most self-test kits require either a nasal swab or a saliva sample.
If a positive result is received, it is important to follow CDC guidelines and isolate. Inform a healthcare professional of the results, and be sure to let close contacts know.
Exploring Vancouver's Airport Accessibility and Options
You may want to see also

On-site testing facilities can produce results in two hours
On-site testing facilities at airports can produce results in as little as two hours. This is a crucial step in reducing the risk of an infected person boarding a plane and passing the virus to others. However, it is important to note that testing is not 100% accurate and even with testing, the risk of infection cannot be completely eliminated. Testing facilities at airports can take the form of pop-up clinics or modular testing centres, often in partnership with laboratories. Testing can be done through molecular tests or antigen tests. Molecular tests, which have a lower false-negative rate, detect genetic material from the virus and must be analysed in a lab, while antigen tests can be administered at home and detect certain proteins in the virus.
The benefits of on-site testing are clear. Testing can help to reduce the spread of the virus and also provides peace of mind for travellers. Testing before boarding can also help travellers avoid quarantine requirements at their destinations. However, it is important to consider the potential drawbacks. Testing facilities may not have the capacity to test all passengers, and if enough tests are produced, the process of testing could create added gridlock at airports. Furthermore, passengers who test negative before travelling may still contract the virus in the days between the test and their flight.
Overall, while on-site testing facilities at airports can produce rapid results and help to reduce the risk of infection, they should be used in conjunction with other safety measures such as mask-wearing and physical distancing.
Lockers at Auckland Airport: Available and Accessible?
You may want to see also
Frequently asked questions
Some of the methods used to detect coronavirus at airports include thermal cameras, temperature checkpoints, and symptom questionnaires.
Thermal cameras are controversial and not always effective at detecting early signs of infection. They may flag passengers with a different type of infection and miss those who are incubating the virus but have not started showing symptoms.
Airport screening has limited effectiveness in detecting infected travellers. A study estimated that 46% of infected travellers would not be detected, depending on the incubation period, sensitivity of screening, and the proportion of asymptomatic cases.
Alternatives to airport screening include providing information to travellers on seeking care if symptoms develop, contact tracing, and implementing quarantine measures.
Testing passengers at airports may not be feasible due to limited testing supplies and the time required for testing, which could create added gridlock. Testing is also not 100% accurate and may not detect the virus in all infected individuals.